This blog is about mastering Parkinson’s Disease Medication for a disease that is mainly a neurological condition that affects millions of people worldwide. This Ultimate guide will help you manage this progressive disorder that primarily impacts movement but can also affect other aspects of a person’s life. The symptoms of Parkinson’s disease can significantly impact a person’s quality of life, making it difficult to perform daily tasks and enjoy activities they once loved.
While there is currently no cure for Parkinson’s disease, there are various treatment options available to help manage the symptoms and improve quality of life. These treatments include traditional medications, advanced treatment options, and lifestyle and supportive therapies. Understanding these treatment options is essential for individuals with Parkinson’s disease and their caregivers to make informed decisions about their healthcare
Parkinson’s disease is a neurodegenerative disorder that primarily affects the nerve cells in a specific part of the brain called the substantia nigra. These nerve cells are responsible for producing a neurotransmitter called dopamine, which plays a crucial role in controlling movement. With Parkinson’s disease, these cells gradually degenerate, leading to a dopamine deficiency in the brain.
The lack of dopamine results in the characteristic symptoms of Parkinson’s disease, including tremors, stiffness, bradykinesia (slowness of movement), and postural instability. These symptoms can vary in severity from person to person and can greatly impact a person’s ability to perform everyday tasks.
In addition to motor symptoms, Parkinson’s disease can also cause non-motor symptoms, such as cognitive impairment, mood changes, sleep disturbances, and autonomic dysfunction. These non-motor symptoms can significantly impact a person’s overall well-being and quality of life.
The symptoms of Parkinson’s disease can vary from person to person, but the most common symptoms include tremors, stiffness, slowness of movement, and balance problems. These motor symptoms typically start on one side of the body and gradually progress to both sides as the disease progresses.
Diagnosing Parkinson’s disease can be challenging, as there is no specific test to confirm the condition. Healthcare providers rely on a combination of medical history, physical examination, and the presence of characteristic symptoms to make a diagnosis. They may also order additional tests, such as imaging scans or blood tests, to rule out other conditions that may cause similar symptoms. However, early diagnosis of Parkinson’s disease is essential, as it allows for early intervention and treatment.
Parkinson’s disease is a progressive disorder, meaning that symptoms worsen over time. The progression of the disease can vary from person to person, with some individuals experiencing a slow progression and others experiencing a more rapid decline in function.
Parkinson’s disease is often classified into stages to help understand the progression of symptoms. The stages range from Stage 1, which represents mild symptoms on one side of the body, to Stage 5, which represents severe symptoms affecting both sides of the body and impairing balance and mobility.
As the disease progresses, individuals may experience increased difficulty with movement, including walking, balance, and coordination. They may also experience more significant motor symptoms, such as freezing episodes, tremors, and stiffness. It is important for individuals with Parkinson’s disease to work closely with their healthcare provider to monitor the progression of their symptoms and adjust treatment accordingly.
Traditional medications are an essential part of the treatment plan for Parkinson’s disease. These medications aim to increase dopamine levels in the brain or mimic its effects to alleviate the motor symptoms of the disease.
The most commonly prescribed Parkinson’s disease medication is levodopa, which is converted into dopamine in the brain. Levodopa is often combined with other medications, such as carbidopa, to enhance its effectiveness and reduce side effects.
Dopamine agonists are another class of medications used to treat Parkinson’s disease. These medications directly stimulate dopamine receptors in the brain, mimicking the effects of dopamine. Common dopamine agonists include pramipexole and ropinirole.
MAO-B inhibitors and COMT inhibitors are other classes of medications used in Parkinson’s disease treatment. MAO-B inhibitors block the enzyme that breaks down dopamine in the brain, while COMT inhibitors prevent the breakdown of levodopa. Examples of MAO-B inhibitors include selegiline and rasagiline, while entacapone is a common COMT inhibitor.
Levodopa is considered the gold standard medication for treating Parkinson’s disease. It is a precursor to dopamine and is converted to dopamine in the brain. Levodopa helps replenish the dopamine levels in the brain, alleviating the motor symptoms of the disease.
One of the benefits of levodopa is its effectiveness in improving motor symptoms, especially in the early stages of Parkinson’s disease. It can significantly reduce tremors, stiffness, and slowness of movement, allowing individuals to regain better control over their motor function.
However, Levodopa is not without its side effects. Common side effects of levodopa include nausea, dizziness, Dysgeusia, and low blood pressure. Some individuals may also experience dyskinesias, which are involuntary movements, as a side effect of long-term levodopa use.
Despite the potential side effects, levodopa remains an essential medication in the treatment of Parkinson’s disease, and healthcare providers carefully monitor its dosage and use to provide the maximum benefit while minimizing side effects.
Dopamine agonists are a class of medications used in the treatment of Parkinson’s disease. These medications directly stimulate dopamine receptors in the brain, mimicking the effects of dopamine.
Dopamine agonists work by binding to specific dopamine receptors, activating them and promoting dopamine-like effects in the brain. This helps alleviate the motor symptoms of Parkinson’s disease, such as tremors, stiffness, and bradykinesia.
While dopamine agonists can be effective in managing the symptoms of Parkinson’s disease, they are also associated with certain side effects. Common side effects of dopamine agonists include nausea, dizziness, and orthostatic hypotension (low blood pressure upon standing). In some cases, dopamine agonists can also cause hallucinations, confusion, and impulse control disorders.
MAO-B inhibitors are a class of medications used in the treatment of Parkinson’s disease. These medications work by inhibiting the enzyme called monoamine oxidase-B (MAO-B), which breaks down dopamine in the brain.
By inhibiting MAO-B, these medications help preserve the levels of dopamine in the brain, improving motor symptoms and overall function in individuals with Parkinson’s disease. MAO-B inhibitors are often used in combination with levodopa to enhance its effectiveness and prolong its duration of action.
Commonly prescribed MAO-B inhibitors include selegiline and rasagiline. These Parkinson’s disease medications have been shown to improve motor symptoms and quality of life in individuals with Parkinson’s disease.
While generally well-tolerated, MAO-B inhibitors can also cause side effects such as nausea, headache, Xerostomia (Dry Mouth) and insomnia. It is important for individuals taking MAO-B inhibitors to work closely with their healthcare provider and report any concerning symptoms or side effects.
COMT inhibitors are a class of medications used as adjunct therapy in Parkinson’s disease medications and treatment. These medications work by inhibiting the enzyme catechol-O-methyltransferase (COMT), which breaks down levodopa in the bloodstream.
By inhibiting COMT, these medications help prolong the effects of levodopa, enhancing its effectiveness in managing motor symptoms. COMT inhibitors are often prescribed in combination with levodopa therapy to optimize symptom control.
Commonly used COMT inhibitors include entacapone and opicapone. These medications can be particularly beneficial in individuals experiencing motor fluctuations or wearing-off symptoms with levodopa therapy.
Side effects of COMT inhibitors may include nausea, diarrhea, and abdominal pain. It is important for individuals taking COMT inhibitors to work closely with their healthcare provider and report any concerning symptoms or side effects.
In addition to traditional medications, there are advanced treatment options available for individuals with Parkinson’s disease. These treatments are typically reserved for individuals who do not achieve optimal symptom control with medication alone or experience medication-related side effects.
One such advanced treatment option is deep brain stimulation (DBS), a surgical procedure that involves implanting electrodes into specific areas of the brain. These electrodes deliver electrical impulses to modulate abnormal brain activity and alleviate motor symptoms. DBS has been shown to be effective in improving motor function and reducing medication requirements in individuals with Parkinson’s disease.
Non-oral therapies, such as patches and injections, are also emerging as alternative treatment options for Parkinson’s disease. These therapies can provide more consistent drug delivery and help manage motor fluctuations.
Deep brain stimulation (DBS) is a surgical procedure used to treat Parkinson’s disease and other movement disorders. It involves implanting electrodes into specific areas of the brain, such as the subthalamic nucleus or globus pallidus. These electrodes deliver electrical impulses to modulate abnormal brain activity and alleviate motor symptoms.
DBS can be highly effective in improving motor function and reducing medication requirements in individuals with Parkinson’s disease. It can help alleviate tremors, stiffness, and dyskinesias, allowing individuals to regain better control over their movements.
The DBS procedure typically involves two surgeries – one to implant the electrodes and another to implant a pulse generator (similar to a pacemaker) in the chest area. The stimulation parameters can be adjusted by healthcare providers to optimize symptom control.
Non-oral therapies are emerging as alternative treatment options for Parkinson’s disease. These therapies provide more consistent drug delivery and can help manage motor fluctuations and dyskinesias. Some examples of non-oral therapies include:
Non-oral therapies can help individuals achieve more consistent symptom control and reduce medication-related side effects, such as fluctuations in motor function and dyskinesias. They can be particularly beneficial for individuals who have difficulty swallowing or experience gastrointestinal issues.
It is important for individuals considering non-oral therapies to work closely with their healthcare provider to determine the most suitable option and adjust the treatment plan as needed.
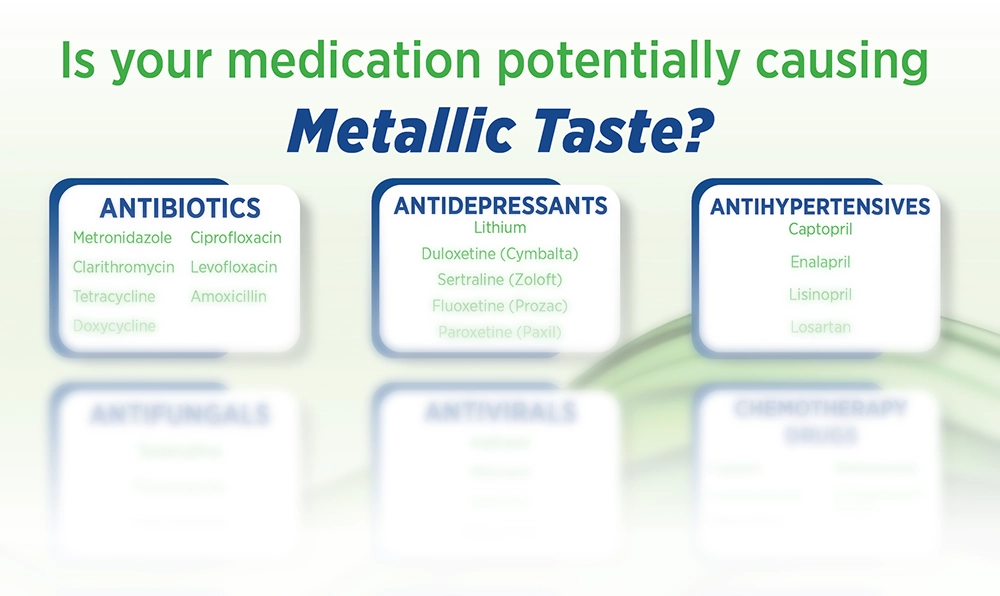
Parkinson’s drugs help with symptoms but can have side effects like nausea, dizziness, and hallucinations. Other side effects can also be Dysgeusia and Xerostomia, that may cause an oral health issue while you are on the medications. Knowing is half the battle, with OTC products that can give you relief from the symptoms, you can plan ahead and take back control of your oral health.
Common side effects of Parkinson’s disease medications can vary depending on the specific medication and individual response. Some of the common side effects include:
It is important for individuals with Parkinson’s disease to discuss any side effects with their healthcare provider, as they can often be managed or mitigated with adjustments to the treatment plan.
Managing side effects and improving quality of life are important aspects of Parkinson’s disease medication. Here are some strategies to help:
Some individuals taking Parkinson’s disease medications may experience a metallic taste as a side effect. This side effect can occur due to changes in taste perception or the medication’s interaction with taste receptors.
If you experience a metallic taste from your medication, it is important to know there is one product out there that can help you find some relief. The first of its kind product, MetaQil is an oral rinse that gently alleviates any unusual taste in the mouth and restores a normal sense of taste. MetaQil has a very mild flavor and does not burn the mouth like typical mouthwash.
MetaQil contains essential oils that are clinically proven to comfort taste disorders. These ingredients provide relief from metallic taste, bitterness and other unpleasant tastes in the mouth.
Emerging trends in Parkinson’s disease treatment hold promise for advancing our understanding and management of the condition. Some of these trends include:
It is important to note that these emerging trends are still under investigation and not yet widely available. Individuals interested in these treatment options should consult with their healthcare provider and consider participating in clinical trials when appropriate.
Gene therapy is an emerging treatment approach for Parkinson’s disease that involves introducing specific genes into the brain to restore or enhance the function of dopamine-producing cells.
With gene therapy, a modified virus is used as a vector to deliver the therapeutic genes into the brain. These genes can help regulate dopamine production, reduce inflammation, or provide neuroprotection to the affected cells.
Early research into gene therapy for Parkinson’s disease has shown promising results, with some studies reporting improved motor function and symptom relief. However, gene therapy is still in the experimental stage and not yet widely available.
Researchers are continuing to explore different gene therapy approaches and develop new drugs and delivery methods to optimize the effectiveness and safety of this treatment approach. It is an exciting area of research that holds promise for the future of Parkinson’s disease treatment.
Stem cell therapy is an emerging treatment approach for Parkinson’s disease that aims to replace or repair damaged dopamine-producing cells in the brain. Stem cells are undifferentiated cells that have the potential to develop into different types of cells in the body.
The goal of stem cell therapy in treating Parkinson’s disease is to transplant healthy dopamine-producing cells into the brain to replace the damaged ones. This approach holds promise for restoring motor function and improving symptoms.
While stem cell therapy is still in the research stage, there have been promising developments in preclinical and early clinical trials. Researchers are exploring various sources of stem cells, including embryonic stem cells, induced pluripotent stem cells, and adult stem cells.
The future of stem cell therapy for treating Parkinson’s disease will depend on further research and clinical trials to ensure its safety and efficacy. It is an exciting area of research that may offer new treatment options for individuals with Parkinson’s disease in the future.
In addition to Parkinson’s disease medication and advanced treatment options, lifestyle and supportive therapies play a crucial role in managing Parkinson’s disease. These therapies can help improve physical function, emotional well-being, and overall quality of life. Some of the key supportive therapies for Parkinson’s disease include:
Physical therapy is an essential supportive therapy for individuals with Parkinson’s disease. It involves exercises and techniques aimed at improving mobility, balance, and strength.
Exercise and physical therapy can help individuals with Parkinson’s disease manage motor symptoms, reduce stiffness, and enhance physical function. Some of the key benefits of physical therapy include:
Working with a physical therapist who specializes in Parkinson’s disease can provide tailored exercises and strategies to address specific motor symptoms and functional limitations.
Proper nutrition plays an important role in managing Parkinson’s disease. Nutritional advice for individuals with Parkinson’s disease may include:
Nutritional advice may vary depending on an individual’s specific needs, symptoms, and medication regimen. It is important for individuals to work closely with their healthcare team to develop a nutrition plan that supports their overall health and well-being.
In conclusion, understanding Parkinson’s disease and its medication options is crucial for effectively managing the condition. From traditional Parkinson’s disease medications like Levodopa to advanced treatments such as Deep Brain Stimulation, there are various approaches available. Managing side effects and exploring emerging trends like gene therapy and stem cell research offer hope for improved outcomes. Lifestyle choices like physical therapy and proper nutrition also play a significant role in enhancing quality of life. Stay informed, consult healthcare professionals, and explore the evolving landscape of Parkinson’s treatment for optimal care.
The best medication for Parkinson’s disease varies depending on individual factors and symptom presentation. It is important to work closely with a healthcare provider to determine the most suitable medication or combination of medications that provide optimal symptom control while minimizing side effects and improving quality of life.
While there is currently no cure for Parkinson’s disease, certain treatment options and lifestyle changes can help slow down the progression of the disease and manage symptoms. Early intervention, regular exercise, a balanced diet, and adherence to medication regimens are important factors in potentially slowing down the progression of Parkinson’s disease.
Supporting someone with Parkinson’s disease involves understanding their needs, providing emotional support, and assisting with daily activities. It is important for family members to educate themselves about the disease, communicate openly, and involve healthcare professionals when needed to ensure the best possible care and support for their loved one.